
Dr. Erika Massicotte
Ophthalmologist specializing in Oculoplastic Surgery
Centre Hospitalier de l’Université de Montréal (CHUM)
As an ophthalmologist specializing in oculoplastic surgery, Dr. Massicotte manages diseases of the structures around the eyes and performs many types of surgeries on the eyelids, the orbit, and the lacrimal system (the network of tear glands and ducts). Dr. Massicotte tailors her approach to each patient’s unique needs to give them the best medical and surgical care possible.
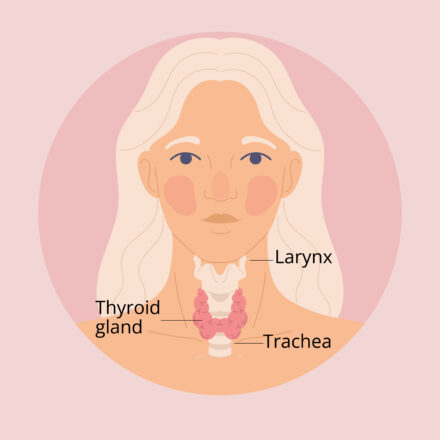
What is the thyroid gland and what does it do?
The thyroid is a small, butterfly-shaped gland at the base of the neck. It releases hormones that are essential for controlling growth and metabolism throughout the body.
Thyroid disease occurs when the thyroid is not functioning properly. A poorly functioning thyroid may be overactive (hyperthyroidism) or underactive (hypothyroidism); either condition can cause wide-ranging health issues. It’s estimated that 1 in 10 Canadians suffers from a thyroid condition.
What is thyroid eye disease (TED)?
Thyroid eye disease is an autoimmune condition. About 90% of cases occur in people with a form of hyperthyroidism called Graves’ disease, but it can also occur in people with low or normal thyroid levels. Once TED has developed, it’s a lifelong condition.
TED has two distinct stages: active and inactive. The active phase of TED is characterized by inflammation. Antibodies released by the thyroid gland attack the muscles and tissues surrounding the eyes, causing them to swell and enlarge. This is when common signs and symptoms of TED, like swelling, redness, and retraction of the eyelids, may first appear and continue to progress. The active stage of TED can last from 1 to 3 years.
“In the active phase, that’s when your appearance will change. It’s important to consult an ophthalmologist as fast as possible because that’s when medication can stop the progression and sometimes even reverse some of the changes the disease has caused.”
Once the disease transitions to an inactive stage, inflammation is replaced by fibrosis/scarring and symptoms become more stable. However, changes to the eyes that occurred during the active phase have a tendency to persist. It’s also possible for the disease to reactivate. Factors that increase the risk of reactivation include:
- Uncontrolled thyroid hormone (levels outside of normal range)
- Smoking
- High cholesterol
- The use of radioactive iodine; while an effective treatment for hyperthyroidism, it’s usually avoided in patients with moderate-to-severe TED. Radioactive iodine may sometimes be used very carefully in patients with mild, inactive TED.
What are the main signs and symptoms of TED?
When the tissues around the eyeball enlarge and swell, it can cause changes to how the eyes look and feel. In addition to putting eye health at risk, these symptoms can have a significant impact on a patient’s quality of life and self-confidence.
Symptoms of TED may include:
- Puffy eyelids – due to increased fat volume in the eyelids
- Eyelid retraction – the muscles in the eyelids can become overactive, causing the eyelids to pull back, so more of the white of the eye is visible
- Eye protrusion – increased fat and swelling in the muscle around the eye push the eye forward
- Dry eye – itchy, burning, or foreign body sensation, blurry vision, and/or red eyes
- Double vision – when the muscles become enlarged and thickened, the eyes can become misaligned (known as strabismus)
- Pain/pressure behind the eye – which is worse when moving the eye
- Vision loss

A TED patient with eye protrusion and retraction of the lower eyelid on both eyes.
I’ve just been diagnosed with Graves’ disease. Does that mean I’ll get TED?
A diagnosis of Graves’ disease doesn’t necessarily mean you will develop TED. Approximately 20-50% of people with Graves’ disease develop eye symptoms, and they typically appear within 12-18 months of diagnosis of thyroid dysfunction. People who smoke and those with a family history are more likely to develop TED.
Most of the patients with TED I see in my practice are women in their 20s to 40s. However, when TED affects older men, the disease tends to be more severe and more difficult to treat, especially in smokers (including those who smoke marijuana or vape).
How is TED treated?
Treatment typically depends on the stage of disease (active or inactive) and on the severity (mild, moderate, or severe).
Mild TED is typically managed with supportive treatment consisting of eye lubrication (e.g., eyedrops or ointment) and selenium supplements for 6 months.
In moderate to severe cases, treatment during the active stage of the disease can stop the progression of symptoms and in some cases, partially reverse the changes.
Medications used to treat TED during the active stage include:
- Systemic corticosteroids (usually given intravenously)
- Radiation therapy
- Immunosuppressants (e.g., rituximab or tocilizumab)

Many targeted therapies that act directly on the inflammatory pathways involved in TED are currently in development and are being studied in clinical trials. Tepezza® (teprotumumab-trbw) is the first such therapy approved in the US for the treatment of TED. As of September 2025, it has been approved by Health Canada, but it has not received a recommendation for public reimbursement from Canada’s Drug Agency (CDA-AMC).
Once TED has reached the inactive stage, reconstructive surgery may be needed to help improve the appearance of the eyes or manage other bothersome symptoms. Surgery can greatly improve a patient’s self-confidence and quality of life.
In an orbital decompression surgery, the bones of the eye socket are broken. Fat may also be removed from the eye socket. This procedure provides more space for the eyes to return to their normal position. Surgery can also be performed to help correct double vision (strabismus surgery) and eyelid retraction (eyelid retraction surgery).
Some targeted therapies (teprotumumab-trbw and tocilizumab) are also being studied for use during the inactive phase of TED.
“Patients with TED see their appearance change quickly and drastically. Treating them medically and surgically can make them feel like themselves again. Helping to give them back their self-confidence is extremely rewarding.”
Can TED lead to permanent vision loss?
Vision loss occurs in about 5% of patients with TED. There are two main causes of vision loss: severe exposure keratopathy and compressive optic neuropathy.
- Exposure keratopathy
When eyelid retraction or eye protrusion (proptosis) prevents the eyelids from closing properly, the cornea can become damaged. Serious conditions like corneal erosion, corneal ulcer, or corneal perforation can cause scarring and permanent vision loss. Severe exposure keratopathy is treated with aggressive ocular lubrication and TED medication. If these aren’t enough, orbital decompression surgery or eyelid retraction surgery may be needed. - Compressive optic neuropathy
Occasionally, swelling of the extraocular muscles can cause compression of the optic nerve, which is the nerve that connects your eye to your brain. This is a serious complication that can result in blindness.
Signs of a possible optic neuropathy include:- Changes in visual acuity
- Changes in colour vision
- A spot in the visual field
If you have TED and notice these symptoms, contact your ophthalmologist immediately. Intravenous steroids need to be started immediately to reduce inflammation. If it doesn’t respond to steroids or other medical therapies, orbital decompression surgery needs to be performed urgently in order to prevent permanent vision loss.
I’ve been diagnosed with TED. How can I be proactive in managing my condition?
The first step is to keep your thyroid hormone levels controlled, as poorly controlled thyroid levels can result in worse eye disease outcomes. Your endocrinologist will prescribe medication to control your thyroid levels. Good communication between your endocrinologist and ophthalmologist is key to achieving the best possible outcomes.
The most important lifestyle change you can make is to stop smoking (including tobacco, marijuana, and vaping) and avoid exposure to second-hand smoke. If you have high cholesterol, follow your doctor’s recommendations (lifestyle and medication) to lower cholesterol levels.

“Smoking is really bad when you have thyroid eye disease. Smoking makes TED more severe and less responsive to treatment.”
Other simple habits can be helpful for managing symptoms of TED:
- Use artificial tears to help relieve dryness and make the eyes feel more comfortable
- Cool compresses, salt restriction, and sleeping with your head elevated may help reduce puffiness and swelling around the eyes
- Wear sunglasses to help with light sensitivity
- Find ways to manage stress (e.g., exercise, proper sleep, meditation, etc.), as stress can exacerbate TED
Visit The Eye Atlas to learn more about the parts of the eye discussed in this article.
