Orthoptics

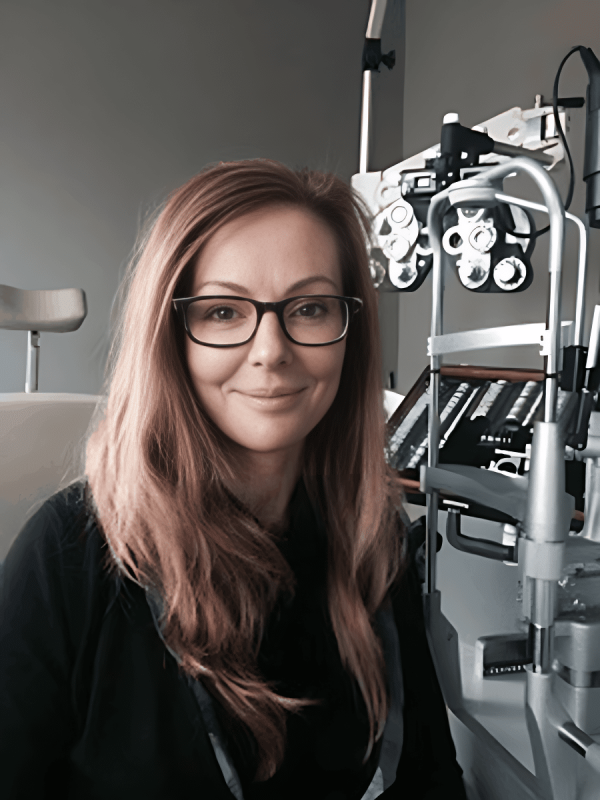
Annick Fournier, MD, FRCSC
Ophthalmologist
Children’s Hospital of Eastern Ontario, University of Ottawa Eye Institute, Ottawa, ON
Dr. Fournier is a practicing ophthalmologist specializing in pediatric ocular surgery and the management of complex pediatric and adult strabismus. She is also involved in medical education, helping to train the next generation of Canadian ophthalmologists. Dr. Fournier currently serves as the President of the Canadian Orthoptic Council (COC).
As an ophthalmologist, I believe that great eye care is all about teamwork. Each member of the eye care team brings their own expertise and skills to the table to support long-term eye health for our patients. You might not have heard of orthoptists, but they’re key players on the eye care team. I’m excited to share more about the orthoptist’s role and the impact they have on our patients’ vision and overall quality of life.

Vaishali Mehta, OC(C)
Orthoptist
Alberta Children’s Hospital, Calgary, Alberta
Vaishali has been practicing orthoptics since 1998. She began her career in the UK before being certified as a Canadian Orthoptist in 2008. She was a member of The Canadian Orthoptic Society (TCOS) executive board between 2010 and 2016, which included a term serving as TCOS President. Vaishali was a faculty member of the Vancouver Orthoptic education program for over a decade and has been Vice President of COC since 2017. She currently lives in Calgary, Alberta and continues to work as a clinical orthoptist.
What is an orthoptist?
Orthos
which means ‘straight’
Optikas
which means ‘relating to sight or vision’

An orthoptist is an allied eye care professional specialized in the visual system.
Orthoptists have a deep understanding of the eye movement systems needed to navigate the world around us and the brain’s ability to interpret vision.

Orthoptists’ specialized education and training sets them apart from other eye care professionals. After earning an undergraduate university degree, orthoptic students complete a 2-year education program that involves extensive clinical experience. They are then required to pass a national exam to become a certified orthoptist in Canada.
A Canadian orthoptist can take on many roles – clinician, educator, researcher, or administrator – to optimize delivery of quality eye health services.
Orthoptists play a key role in assessing, diagnosing, and treating problems with vision related to:
Eye movement
Eye alignment
Binocular vision
(how the eyes work together)
“Orthoptists’ unique training and experience allows us to identify a patient’s cause of visual difficulties and formulate a treatment plan to improve their vision and quality of life. As patient advocates, we listen to our patients and their families to understand their needs, goals, and daily routines. Taking the time to consider the patient’s input allows us to plan and adapt treatment so it is practical and achievable.” – Vaishali Mehta
While best known for their expertise in children’s eye disorders, orthoptists provide care over the entire human lifespan.

Orthoptics was pioneered in the 1920s by Mary Maddox, who used her knowledge of eye movement to help her father, an ophthalmologist. Since then, orthoptists have continued to work alongside ophthalmologists and within multidisciplinary groups to provide eye care to patients. They’ve also made key contributions to research that have advanced our understanding of ocular motility.

What conditions do orthoptists help treat?
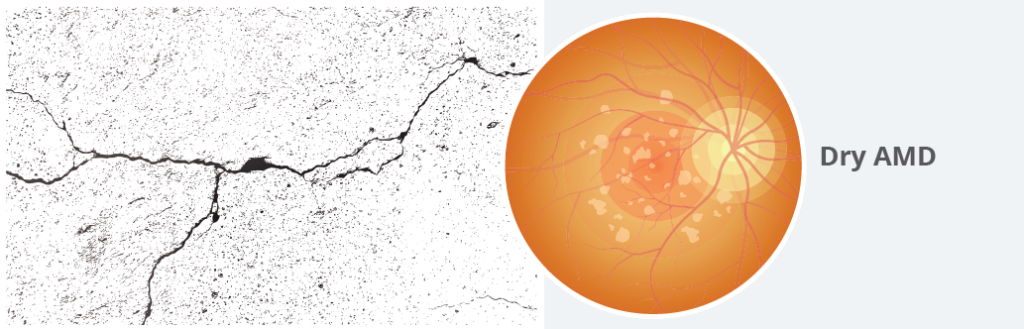
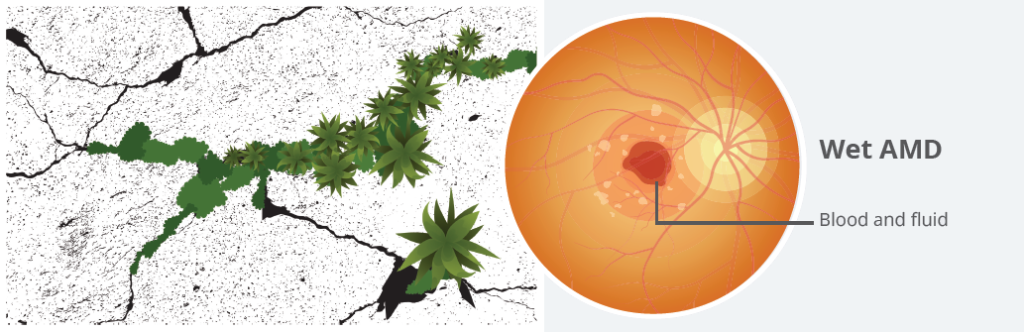
Strabismus and amblyopia
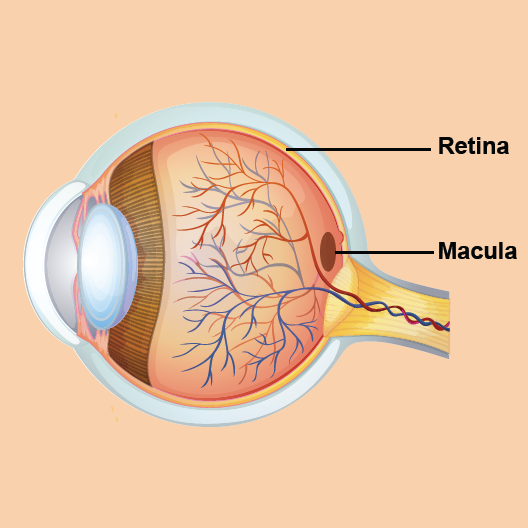
Strabismus refers to any misalignment of the eyes (sometimes referred to as “crossed eyes”). It’s a common cause of amblyopia (when the brain favours one eye, leading to reduced vision in the other).
Orthoptists carry out examinations of eye movement in patients of all ages with strabismus, including those who have developed strabismus as adults. These screenings help to uncover underlying causes of strabismus and how the condition is affecting the patient’s vision. While most cases of strabismus are not caused by serious health issues, orthoptists are trained to recognize when the condition may be a sign of something more concerning, such as a stroke or brain tumour. When such causes are suspected, orthoptists can quickly triage these patients to be seen urgently.

Orthoptists focus on non-surgical treatment of strabismus and amblyopia using glasses or patching to help strengthen the vision of the weaker eye. When glasses are prescribed by the ophthalmologist, the orthoptist makes suggestions for adjusting the glasses prescription to ensure the patient has clear and comfortable vision, and to promote binocularity. These treatments are usually started before surgery, and might continue afterward too.

Double vision
Orthoptists are often are called on to assess visual function in adults with double vision. Orthoptists have the skills to determine precisely how the binocular visual system has been affected. This can sometimes help diagnose an underlying medical cause of double vision (like strabismus, a vascular disease, stroke, multiple sclerosis, or a thyroid condition like Graves’ disease).
For patients experiencing double vision, orthoptists can provide treatment to help relieve symptoms. Double vision can often be treated with prism therapy, which relies strongly on the orthoptist’s knowledge of visual principles. Improving visual comfort is crucial, especially for adult patients, to be able to continue to live a more normal life, either while they await strabismus surgery or as an alternative to surgery.
Convergence insufficiency
When we use our near vision for tasks like looking at a smartphone or reading a book, both eyes naturally turn inward to focus on what’s in front of us. Convergence insufficiency is a condition where the eyes don’t converge enough for clear near vision, which can make it difficult to focus on close-up work. It’s fairly common for adults to develop some degree of convergence insufficiency as they get older, and it can show up with symptoms like headaches, double vision, and eye strain while reading. Convergence insufficiency is often present in children and can make reading or doing schoolwork uncomfortable, which might affect how well they focus or learn. While convergence insufficiency isn’t a learning disability, it is sometimes found in children who have been diagnosed with one.
Orthoptists can recommend eye exercises that improve convergence ability and help relieve the symptoms of convergence insufficiency.
How do ophthalmologists and orthoptists work together?
In Canada, practicing orthoptists always work in partnership with ophthalmologists, either in hospitals or private clinics.
Orthoptists play an active role in assessing, diagnosing, and treating many ocular conditions.

Orthoptist

Ophthalmologist
Assessment and Diagnosis
The orthoptist evaluates the patient’s eye function and visual symptoms.
The ophthalmologist checks the health of the structures of the eye through a comprehensive eye exam, visual acuity tests, and imaging.
Together, these assessments allow for a more complete picture of the patient’s visual health so a diagnosis and collaborate treatment plan can be made.
Treatment
The orthoptist manages non-surgical treatment options, such as glasses, patching, or prisms.
The orthoptist’s evaluations provide data for surgical planning and prognosis.
The ophthalmologist provides medical and surgical treatment.

Mason (age 3)
To help understand how ophthalmologists and orthoptists work together, let’s look at Mason’s experience receiving treatment for strabismus and amblyopia.

Mason’s pediatrician refers him to an ophthalmology clinic because his left eye is turned inwards (esotropia)

Within a few weeks of referral, Mason is seen by the clinic’s orthoptist
The orthoptist:
- does a full assessment of how well Mason can see, focus his eyes, and move his eyes together
- suggests a working diagnosis of strabismic amblyopia
- recommends that Mason return for a dilated eye exam with the ophthalmologist within the next month

3 weeks later, Mason returns to the clinic
The orthoptist screens Mason to assess any change since his last visit
The ophthalmologist:
- does a full eye exam, including measuring for any refractive error
- prescribes glasses

Over the next 6 months, Mason returns to the clinic regularly
- ensures that the glasses were made correctly, that the power is right, and that they improve Mason’s vision
- checks in on how Mason is doing with his glasses and offers his parents guidance to encourage wearing them
- prescribes patching treatment to help strengthen the vision in the left eye, teaches his parents how to patch, and shows his parents activities that will help Mason comply with the patching
- monitors Mason’s progress with the patching treatment and makes adjustments to the treatment plan as needed

By his next visit, Mason’s vision has improved to an acceptable level
- recommends surgery to help realign the eyes
- does a full ocular motility exam
- discusses Mason’s progress with his parents
- repeats the full eye exam
- assesses Mason for surgery and confirms it is the appropriate next step

Pre-op visit
- Takes a final set of measurements before surgery
- Answers any questions Mason’s parents have

Mason gets strabismus repair surgery
The ophthalmologist performs surgery to adjust the tension of Mason’s eye muscles to help realign his eyes

A week after surgery, Mason returns to the clinic for a follow-up appointment
The orthoptist recommends that Mason keeps wearing his glasses and continues patching the right eye, with regular follow-up to assess eye alignment and vision
The ophthalmologist checks to ensure Mason’s eyes are healing well after surgery
How do orthoptists improve patient care?
The orthoptist’s expertise helps improve everyday functioning in patients with ocular movement disorders which might be found in childhood or after trauma, stroke, or general health disorders.
For many patients, orthoptists act as the front-line eye care team member. This allows them to:
- Build trust with patients and their families
- Empower patients with support and guidance to follow through on recommended treatment
- Regularly assess progress and tailor the treatment plan as needed

The collaborative approach between orthoptists and ophthalmologists ensures patients get complete, well-rounded eye care:
Orthoptists focus on the functional aspects of vision
Ophthalmologists handle the medical and surgical care
Together, they give patients the best chance possible at healthy vision for life.




























































 Is too much screen time really bad for my kids’ eyes?
Is too much screen time really bad for my kids’ eyes?