Eye Injury
What are eye injuries?
Eye injuries are common and can cause anything from minor scratches to the cornea to vision loss or even blindness. Even if you think an injury is minor or are unsure you have an eye injury, it’s best to get checked out by your eye doctor. In general, anything other than small scratches or grit in the eye may be potentially serious.
Signs of a potentially serious eye injury are:
- Continuous eye pain
- Difficulty seeing
- One eye not moving as well as the other
- Cut/torn eyelid
- One eye sticking further out of its socket
- Unusual pupil size or shape
- Something in the eye that can’t be removed by tears/blinking
- Blood in the clear part of the eye (the clear, dome-shaped area at the front of the eye between your cornea and iris)
Causes
Common causes of eye injuries are:
- Blows to the eye (e.g., from balls or hands)
- Pieces of flying debris from explosions or industrial work
- Darts, fireworks, bullets
- Chemical splashes

Risk Factors
You may be more at risk of getting any eye injury if you:
- Play a sport, particularly a contact sport
- Work in construction or an industrial setting
- Work around chemicals
- Don’t use protective eyewear

Diagnosis
What happened to your eye will determine what tests a doctor uses to make a diagnosis. First, your doctor will need to know exactly what happened to your eye. This will help him or her decide what diagnostic tests to use.
Below are some of the tests an eye doctor may use to make a diagnosis of an eye injury.
Visual acuity test
This test helps your eye doctor see if you’ve had any changes in your vision. You’ll be asked to look at an eye chart with different sizes of letters on it. Your doctor will test one eye at a time, with the other eye covered.
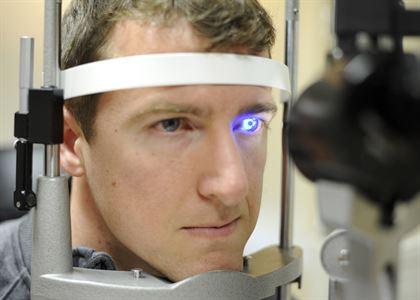
Slit-lamp examination
A slit lamp allows your eye doctor to view different parts of your eye up close to see if there are any problems. This device is called a “slit lamp” because it uses a bright line of light to illuminate the different parts of your eye.
Retinal exam
Your doctor will perform a retinal exam to look for damage in the back part of the eye. Eye drops will be placed into the eyes to widen the pupils. Your doctor will then use a device called an ophthalmoscope to get a good look at your retina.
Fluorescein eye stain test
This test is used to see if you have any scratches on your cornea. Your eye doctor will put drops of a dark orange dye called fluorescein in your affected eye. He or she will then shine a special blue light into your eye. Any areas that are damaged will appear green.
X-ray
In some cases, your doctor may order an X-ray. This will help him or her to see if you have a fracture in your eye bone, or if there are any foreign objects inside your eye.
Ultrasound
If your eye doctor cannot see into the back of the eye, he or she may also order an ultrasound. This test uses high-frequency sound waves to create a picture of structures in the back of the eye.
Treatment
How your eye injury is treated depends on what the injury is and how severe it is. Below are some general guidelines.
Eye Scratches & Corneal Abrasions
Most eye scratches and corneal abrasions are minor and will heal on their own within a few days to a week. Still, if you’ve scratched your eye, it’s a good idea to see your eye doctor. If you’re in a lot of pain or are having difficulty seeing, it is important to have the eye assessed quickly.
Treatments you may be prescribed by your eye doctor include:
• Antibiotic eye drops or ointment to treat infection
• Steroid eye drops to treat inflammation
• Eye drops to lubricate your eyes.
Small Particles in the Eye
Our eyes are good at flushing natural particles like sand or dirt out through tears and blinking. This is usually not an emergency. Man-made particles like metal or glass, however, may be cause for concern. These kinds of particles can stick in the eye and create lasting irritation.
Whatever the particle, if you continue to feel like there’s something in your eye, see your eye doctor or go to your nearest emergency room.
General tips for dealing with particles in your eye:
- Do not rub your eye
- Try to allow your natural tears to flush out the particle; try blinking several times
- Use saline solution or tap water to flush out your eye
Getting Hit in the Eye
If you have a black eye or notice any pain or changes in your vision ‑ even after a slight blow ‑ see your eye doctor or visit the emergency room.
- General tips for managing a blow to your eye:
- Do not put any pressure on your eye
- Apply a cold compress GENTLY to help reduce pain and swelling
Eye Cut or Puncture
If your eye has been cut or punctured, see your eye doctor or get medical attention right away.
Carefully place a protective shield over the eye (e.g., bottom of a paper cup taped to the skin around your eye); be careful not to press the shield directly against the eye.
DO NOT do any of the following:
- Rub your eye or apply pressure to it
- Rinse your eye with water
- Try to remove any objects that are in your eye
- Take aspirin, ibuprofen, naproxen or other non-steroidal anti-inflammatory medications as these may cause you to bleed more
Splashes/Chemical Burns in the Eye
If any chemicals get splashed in your eye or you suffer a chemical burn in your eye, follow these steps:
- Immediately flush your eye with lots of clean water
- Get emergency medical help right away
- Try to find out the name of the chemical—this will help the doctor know how to treat your eye